Meningococcal disease can refer to any illness caused by the type of bacteria called
Neisseria meningitidis, also known as meningococcus [muh-ning-goh-KOK-us]. These illnesses
are often severe and can be deadly. They include infections of the lining of the brain
and spinal cord (meningitis) and bloodstream infections (bacteremia or septicemia).
These bacteria spread through the exchange of respiratory and throat secretions like
spit (e.g., by living in close quarters, kissing). Doctors treat meningococcal disease
with antibiotics, but quick medical attention is extremely important. Keeping up to
date with recommended vaccines is the best defense against meningococcal disease.
Causes
Bacteria called Neisseria meningitidis cause meningococcal disease. About 1 in 10
people have these bacteria in the back of their nose and throat with no signs or symptoms
of disease; this is called being 'a carrier'. But sometimes the bacteria invade the
body and cause certain illnesses, which are known as meningococcal disease.
There are five serogroups (types) of Neisseria meningitidis – A, B, C, W, and Y –
that cause most disease worldwide. Three of these serogroups (B, C, and Y) cause most
of the illness seen in the United States.
People spread meningococcal bacteria to other people by sharing respiratory and throat
secretions (saliva or spit). Generally, it takes close (for example, coughing or kissing)
or lengthy contact to spread these bacteria. Fortunately, they are not as contagious
as germs that cause the common cold or the flu. People do not catch them through casual
contact or by breathing air where someone with meningococcal disease has been.
Sometimes the bacteria spread to people who have had close or lengthy contact with
a patient with meningococcal disease. Those at increased risk of getting sick include:
- People who live with the patient
- Anyone with direct contact with the patient's oral secretions, such as a boyfriend
or girlfriend
Close contacts of someone with meningococcal disease should receive antibiotics to
help prevent them from getting the disease. This is known as prophylaxis (pro-fuh-lak-sis).
Health departments investigate each case of meningococcal disease to identify all
close contacts and make sure they receive prophylaxis. This does not mean that the
contacts have the disease; it is to prevent it. People who are not a close contact
of a patient with meningococcal disease do not need prophylaxis.
Seek medical attention immediately if you develop symptoms of meningococcal disease.
Symptoms of meningococcal disease can first appear as a flu-like illness and rapidly
worsen. The two most common types of meningococcal infections are meningitis and septicemia.
Both of these types of infections are very serious and can be deadly in a matter of
hours.
Meningococcal Meningitis
Doctors call meningitis caused by the bacteria Neisseria meningitidis meningococcal
meningitis. When someone has meningococcal meningitis, the bacteria infect the protective
membranes covering their brain and spinal cord and cause swelling.
The most common symptoms include:
- Fever
- Headache
- Stiff neck
There are often additional symptoms, such as:
- Nausea
- Vomiting
- Photophobia (eyes being more sensitive to light)
- Altered mental status (confusion)
If you think you have any of these symptoms, call the doctor right away.
Meningococcal Septicemia (aka Meningococcemia)
Doctors call septicemia (a bloodstream infection) caused by Neisseria meningitidis
meningococcal septicemia or meningococcemia. When someone has meningococcal septicemia,
the bacteria enter the bloodstream and multiply, damaging the walls of the blood vessels.
This causes bleeding into the skin and organs.
Symptoms may include:
- Fever
- Fatigue
- Vomiting
- Cold hands and feet
- Cold chills
- Severe aches or pain in the muscles, joints, chest or abdomen (belly)
- Rapid breathing
- Diarrhea
- In the later stages, a dark purple rash
If you think you have any of these symptoms, call the doctor right away.
Keeping up to date with recommended immunizations is the best defense against meningococcal
disease. Maintaining healthy habits, like getting plenty of rest and not having close
contact with people who are sick, also helps.
Vaccination
Vaccines help protect against all three serogroups (B, C, and Y) of Neisseria meningitidis
bacteria commonly seen in the United States. Like with any vaccine, meningococcal
vaccines are not 100% effective. This means there is still a chance you can develop
meningococcal disease after vaccination. People should know the symptoms of meningococcal disease since early recognition and quick medical attention are extremely important.
CDC recommends vaccination with a meningococcal conjugate vaccine (ACWY) for all preteens
and teens at 11 to 12 years old, with a booster dose at 16 years old. Teens and young
adults (16 through 23 year olds) also may be vaccinated with a serogroup B meningococcal
vaccine.
Learn more about what everyone should know about meningococcal vaccination.
Antibiotics
Close contacts of a person with meningococcal disease should receive antibiotics to
prevent them from getting sick. This is known as prophylaxis (pro-fuh-lak-sis).
Examples of close contacts include:
- People in the same household or roommates
- Anyone with direct contact with a patient's oral secretions (saliva or spit), such
as a boyfriend or girlfriend
Doctors or local health departments recommend who should get prophylaxis.
Re-Infection
If you get meningococcal disease twice, your doctor should check to see if you have
an underlying immune deficiency.
Although rare, people can get meningococcal disease more than once. A previous infection
will not offer lifelong protection from future infections. Therefore, CDC recommends
meningococcal vaccines for all preteens and teens. In certain situations, children
and adults should also get meningococcal vaccines.
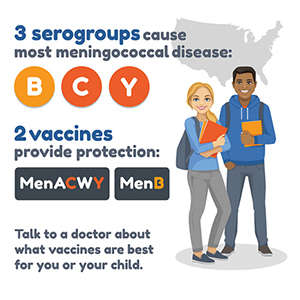 Two meningococcal vaccines (MenACWY and MenB) provide protection against the serogroups
that cause most meningococcal disease in the United States. The Meningitis vaccine
that is required for the traditional undergraduates and residents is Meningitis ACWY,
it does not protect against Meningitis B.
Two meningococcal vaccines (MenACWY and MenB) provide protection against the serogroups
that cause most meningococcal disease in the United States. The Meningitis vaccine
that is required for the traditional undergraduates and residents is Meningitis ACWY,
it does not protect against Meningitis B.